379
Views & Citations10
Likes & Shares
Abbreviation: LSTC: Laparoscopic Subtotal Cholecystectomy; STC: Subtotal Cholecystectomy; OC: Open Cholecystectomy; LC: Laparoscopic Cholecystectomy; ERCP: Endoscopic Retrograde Cholangiopancreatography; CBD: Common Bile Duct; CVS: Critical View of Safety; PC: Partial Cholecystectomy; GB: Gall Bladder
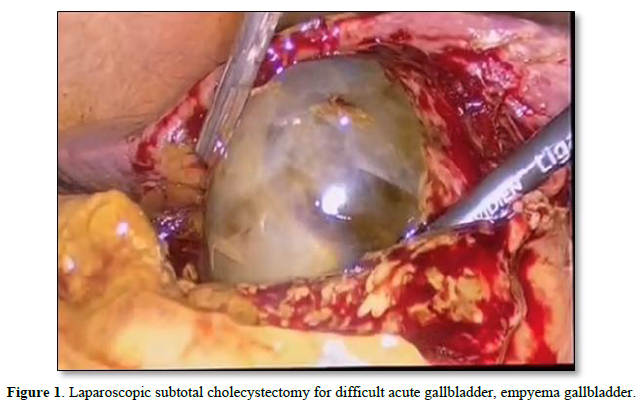
The idea of a partial cholecystectomy, which included removing three-quarters of the gallbladder while keeping a portion of the liver's posterior wall linked to it without electro coagulating the mucosa, was put forth in 1950 [6,7]. In 1985, the operation was enhanced to include a wallet-string strategy for cystic duct closure. Gallbladder removal was made simpler by the open subtotal cholecystectomy technique. Thanks to enhanced laparoscopic capabilities, laparoscopic subtotal cholecystectomy (LSC) has emerged as a feasible alternative for patients with severe acute or chronic cholecystitis, as well as benign gallbladder and biliary disorders [8]. Although conceptually straightforward, this technique may be difficult for surgeons to perform and is often suggested when dissecting Calot's triangle during LC. Laparoscopic partial cholecystectomy (LPC) provides an alternate strategy for preventing bile duct damage, although its safety and effectiveness are questionable [9]. Laparoscopic subtotal cholecystectomy, on the other hand, is a safe, useful, and efficient procedure that could help patients with severe cholecystectomy avoid conversion to open surgery [1,3,4] (Figure 1).
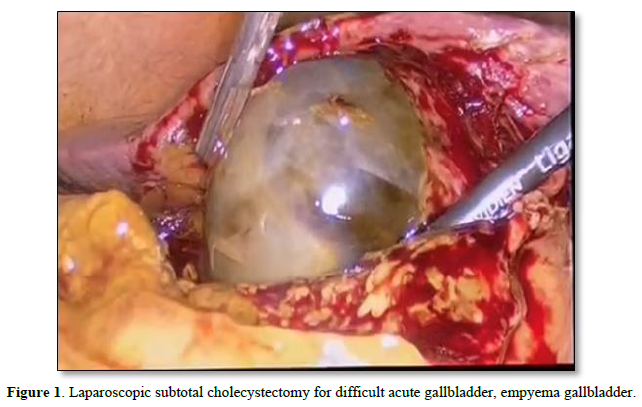
In 1955, Madding made the first suggestion for partial cholecystectomy as a substitute for cholecystostomy and as a last resort when total cholecystectomy proved technically challenging [10,11]. During the surgery, the extra gallbladder wall was removed, and the gallbladder on the fundus was incised to a distance of 1 cm from the cystic duct. Bornman and Terblanche discussed their pleasure with this procedure in dealing with problematic gallbladders linked to severe cholecystitis and portal hypertension thirty years later [11,12] (Figure 2).

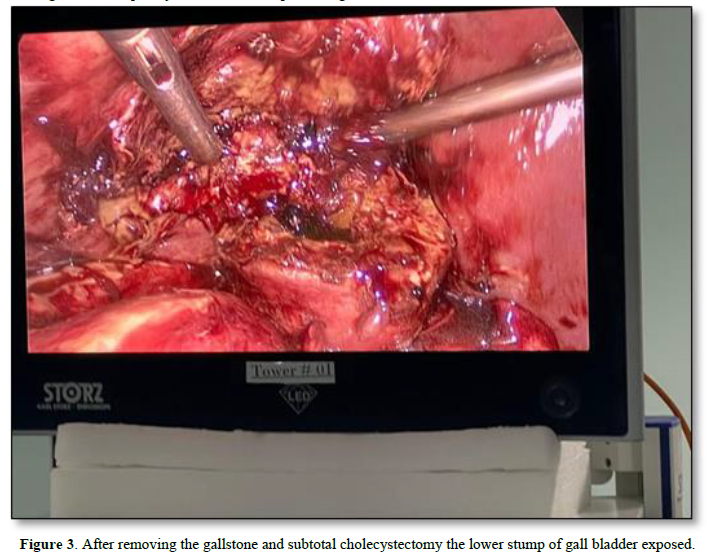
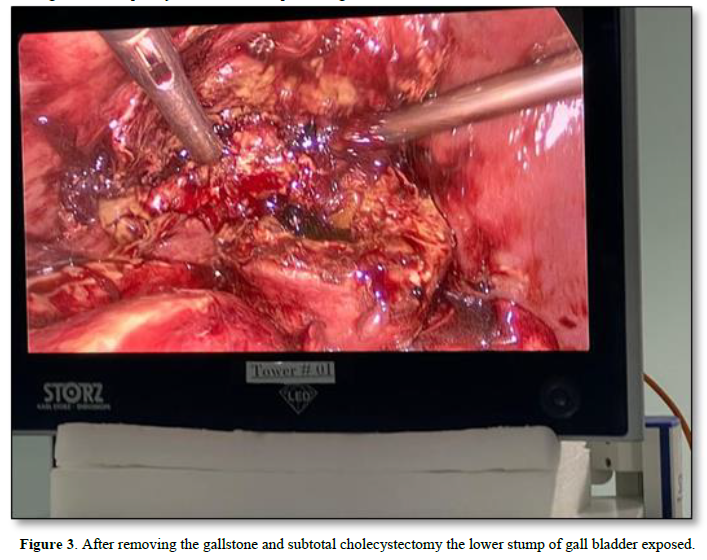
In carefully chosen individuals with severe cholecystectomies, laparoscopic subtotal cholecystectomy is a safe and efficient treatment that may avoid the need for open surgery [13]. The ability to perform a hard-laparoscopic partial cholecystectomy is becoming more and more crucial. A 3-5 times greater chance of bile duct damage occurs during laparoscopy than during open surgery when LC is challenging. The use of this strategy should be carefully considered by surgeons. The "rescue procedure," known as subtotal cholecystectomy (STC), ensures the success of the operation for both the surgeon and the patient [14]. Making decisions quickly is essential for preventing bad results. A difficult cholecystectomy is one that necessitates switching from laparoscopic to open surgery, takes longer than 180 minutes, results in a blood loss of more than 300 ml, and requires prompt help from a more skilled surgeon [15,16]. The Hartmann reservoir is the first part of the gallbladder to be removed, followed by a border of the posterior wall attached to the liver [17]. The cystic duct is sutured shut from the inside of the common bile duct, and the mucous membrane of the residual gallbladder is either coagulated or left intact. This approach has been employed in various ways by surgeons [18] (Figure 3).
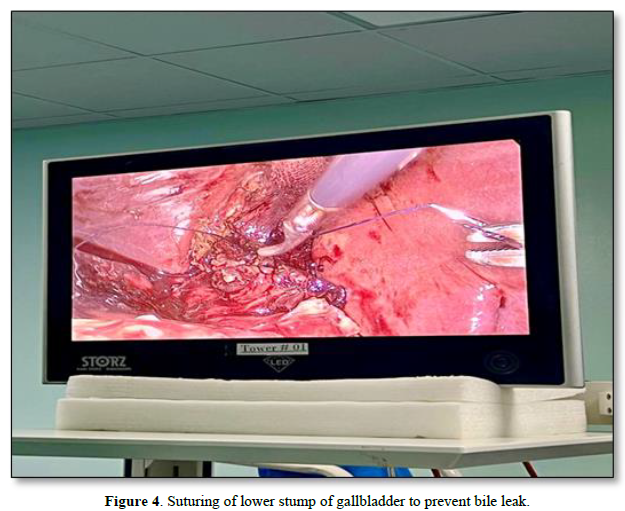
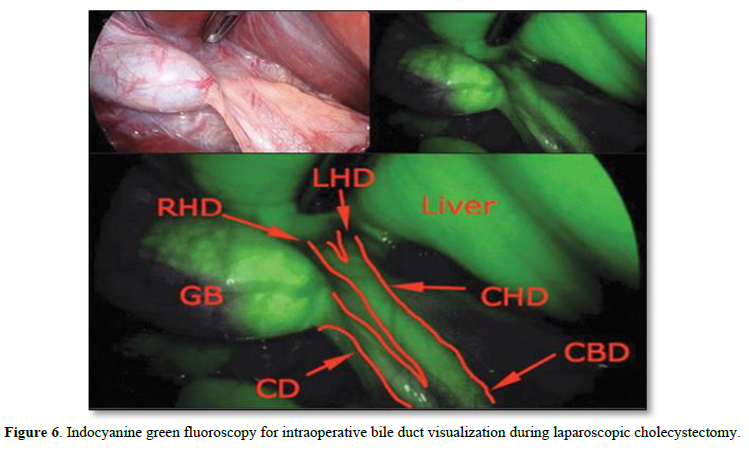
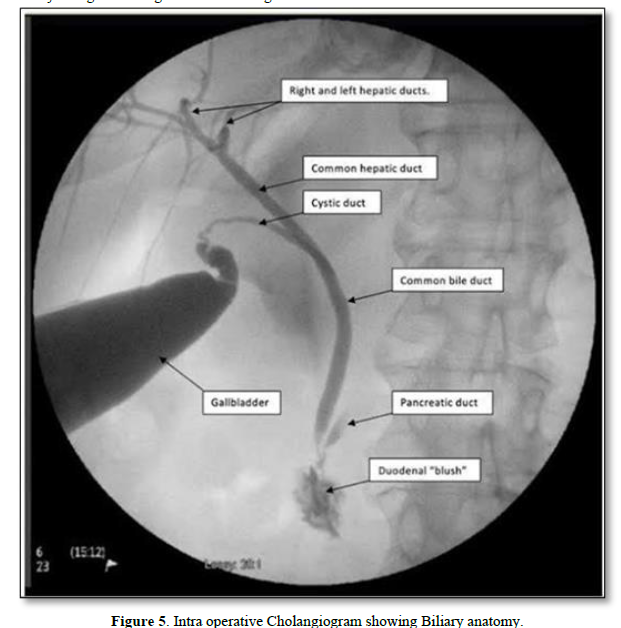
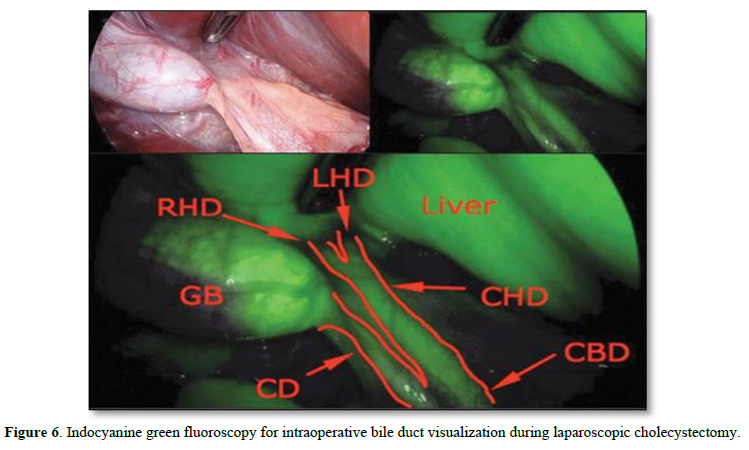
The severity of the illness, the existence of adhesions and anatomical alterations, the surgeon's skill with laparoscopic surgery, and the state of surgical technology are only a few of the variables that might contribute to the difficulties of cholecystectomy [1,4]. Anatomical landmarks may shift as a result of fibrosis brought on by severe inflammation in Calot's triangle, which also raises the possibility of inadvertent harm to the common hepatic duct, common bile duct, and cystic duct [17]. The severity of acute cholecystitis is associated with a greater risk of bile duct injury, which may require liver resection or transplantation, higher hospital expenses, and higher mortality rates. To avoid bile duct damage, surgeons use strategies including getting a critical view of safety (CVS), locating Rouvière's sulcus, conducting an intraoperative cholangiogram (IOC), using an intraoperative fluorescent cholangiogram with indocyanine green, and switching to an open operation [19] (Figure 4).
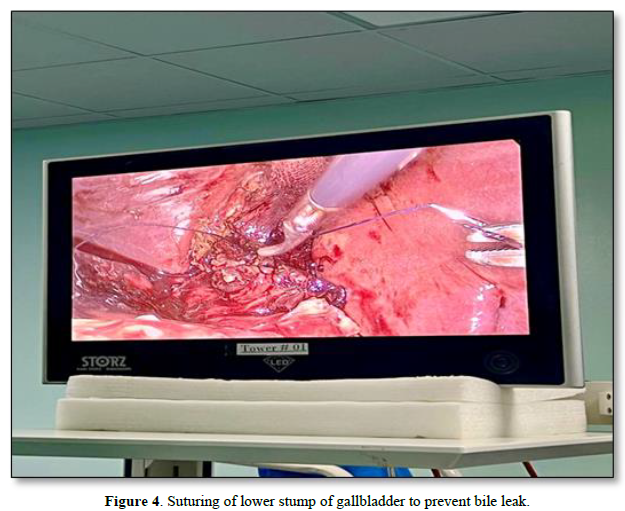
According to recent meta-analyses, the use of indocyanine green fluorescence cholangiography (FC) during surgery lowers bile duct lesions and conversion rates in open surgery much more than the use of only white light cholecystectomy [20]. These methods enable patients to finish their treatment without worrying about long-term consequences [20]. It is suggested to stay away from Calot's triangle and instead choose a partial cholecystectomy if these measures cannot be adopted. Limited data suggests that partial cholecystectomy lowers bile duct damage and conversion rates, but it may also increase bile leakage and retain stones, necessitating further surgery [21]. When portal hypertension or extensive fibrosis impede safe dissection in Calot's triangle, keeping the posterior wall of the gallbladder connected to the liver and closing the cystic duct with a purse-string technique is a potential alternative [11]. The time it takes to stop bleeding from the remaining gallbladder edge is reduced by using a running suture following each stage of gallbladder removal. Appropriate abdominal drainage is necessary after the surgery [22]. In certain circumstances, subhepatic accumulation may happen if the drain is withdrawn too quickly [22]. Reoperation or radiologic intervention may be required in challenging circumstances. It is advisable to keep the posterior wall intact after surgery to reduce leakage and bleeding since inflamed gallbladder walls may induce bleeding. Free bile in the abdomen is often linked to wound infection, and postoperatively, persistent stones in the main bile duct may be seen. These stones may be caused by gallbladder disease or therapy-induced migration [23]. The number of patients who had bile duct stones before surgery was not made clear in the research. Endoscopic retrograde cholangiopancreatography (ERCP), while it sometimes damages the biliary system, is often effective in addressing this issue [17,18,23].
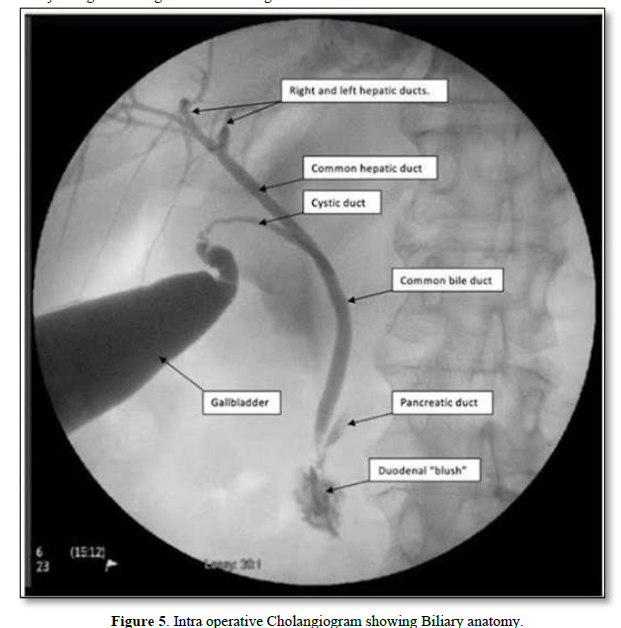
The severity of the illness, the existence of adhesions and anatomical alterations, the surgeon's skill with laparoscopic surgery, and the state of surgical technology are only a few of the variables that might contribute to the difficulties of cholecystectomy [24]. Anatomical landmarks may shift as a result of fibrosis brought on by severe inflammation in Calot's triangle, which also raises the possibility of inadvertent harm to the common hepatic duct, common bile duct, and cystic duct [12]. The severity of acute cholecystitis is associated with a greater risk of bile duct injury, which may require liver resection or transplantation, higher hospital expenses, and higher mortality rates [25]. To avoid bile duct damage, surgeons use strategies including getting a critical view of safety (CVS), locating Rouvière's sulcus, conducting an intraoperative cholangiogram (IOC), using an intraoperative fluorescent cholangiogram with indocyanine green, and switching to an open operation [25].
According to recent meta-analyses, the use of indocyanine green fluorescence cholangiography (FC) during surgery lowers bile duct lesions and conversion rates in open surgery much more than the use of only white light cholecystectomy [26]. These methods enable patients to finish their treatment without worrying about long-term consequences [26]. It is suggested to stay away from Calot's triangle and instead choose a partial cholecystectomy if these measures cannot be adopted. Limited data suggests that partial cholecystectomy lowers bile duct damage and conversion rates, but it may also increase bile leakage and retain stones, necessitating further surgery [27]. When portal hypertension or extensive fibrosis impede safe dissection in Calot's triangle, keeping the posterior wall of the gallbladder connected to the liver and closing the cystic duct with a purse-string technique is a potential alternative [14,18]. The time it takes to stop bleeding from the remaining gallbladder edge is reduced by using a running suture following each stage of gallbladder removal [19]. Appropriate abdominal drainage is necessary after the surgery [18]. In certain circumstances, subhepatic accumulation may happen if the drain is withdrawn too quickly [18]. Reoperation or radiologic intervention may be required in challenging circumstances [18]. It is advisable to keep the posterior wall intact after surgery to reduce leakage and bleeding since inflamed gallbladder walls may induce bleeding. Free bile in the abdomen is often linked to wound infection, and postoperatively, persistent stones in the main bile duct may be seen [17]. These stones may be caused by gallbladder disease or therapy-induced migration. The number of patients who had bile duct stones before surgery was not made clear in the research. Endoscopic retrograde cholangiopancreatography (ERCP), while it sometimes damages the biliary system, is often effective in addressing this issue [17,20,27] (Figures 5 & 6).
Better immediate and long-term results might be achieved by identifying and treating bile duct damage (BDI) during surgery. Endoscopic retrograde cholangiopancreatography (ERCP) is helpful in situations of biliary leakage as well as in removing any remaining stones from the biliary system since these stones may raise pressure in the main bile duct and, if left open, can leak from the cystic duct [28]. ERCP has effectively corrected these issues in 95% of instances [28]. Biliary leakage is the most frequent result of partial resection of the gallbladder wall in patients with severe acute cholecystectomy who are being treated with subtotal cholecystectomy [29]. This disease has a comparatively low fatality rate. According to our research, the most common reason for biliary leakage is leaving the gallbladder wall exposed. Therefore, this procedure should only be used as a last option to treat such individuals [27,28]. ERCP or stent implantation may be used to treat a variety of biliary leakage conditions, however these procedures are more expensive and have a negative impact on patients' quality of life since they need frequent outpatient visits [29].
The majority of subhepatic fluid collections are not infectious, however an abscess may sometimes be found. Some of these aggregates could be reabsorbed with no negative effects on health. Emergency general surgery has been added to damage control surgery, which was initially created for trauma-related diseases. In this work, we developed a damage control technique for cholecystectomy, one of the most common surgical operations [27,28]. A laparoscopic subtotal fenestrating cholecystectomy is carried out on a patient with acute cholecystitis when considerable intraoperative inflammation is seen. In challenging circumstances or when gallbladder cancer is suspected, conversion to open surgery is regarded as a practical approach [30,31].
- Blum CA, Adams DB (2011) Who did the first laparoscopic cholecystectomy? J Minim Access Surg 7: 165-168.
- Wiseman JT, Sharuk MN, Singla A, Cahan M, Litmin DE, et al. (2010) Surgical management of acute cholecystitis at a tertiary care center in the modern era. Arch Surg 145: 439-444.
- Buddingh KT, Hofker HS, Ten Cate Hoedemaker HO, van Dam GM, Ploeg RJ, et al. (2011) Safety measures during cholecystectomy: Results of a nationwide survey. World J Surg 35: 1235-1241.
- Dissanaike S (2016) A Step-by-Step Guide to Laparoscopic Subtotal Fenestrating Cholecystectomy: A Damage Control Approach to the Difficult Gallbladder. J Am Coll Surg 223(2): e15-8.
- Nakajima J, Sasaki A, Obuchi T, Baba S, Nitta H, et al. (2009) Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg Today 39: 870-875.
- Singhal T, Balakrishnan S, Hussain A, Nicholls J, Grandy-Smith S, et al. (2009) Laparoscopic subtotal cholecystectomy: Initial experience with laparoscopic management of difficult cholecystitis. Surgeon 7(5): 263-268.
- Macaron C, Qadeer MA, Vargo JJ (2011) Recurrent abdominal pain after laparoscopic cholecystectomy. Cleve Clin J Med 78: 171-178.
- Maehira H, Kawasaki M, Itoh A, Ogawa M, Mizumura N, et al. (2017) Prediction of difficult laparoscopic cholecystectomy for acute cholecystitis. J Surg Res 216: 143-148.
- Katsohis C, Prousalidis J, Tzardinoglou E, Michalopoulos A, Fahandidis E, et al. (1996) Subtotal cholecystectomy. HPB Surg 9: 133-136.
- Di Carlo I, Pulvirenti E, Toro A, Corsale G (2009) Modified subtotal cholecystectomy: Results of a laparotomy procedure during the laparoscopic era. World J Surg 33: 520-525.
- Jeong IO, Kim JY, Choe YM, Choi SK, Heo YS, et al. (2011) Efficacy and feasibility of laparoscopic subtotal cholecystectomy for acute cholecystitis. Korean J Hepatobiliary Pancreat Surg 15: 225-230.
- Beldi G. Glättli A (2003) Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg Endosc 17: 1437-1479.
- Özçınar B, Memişoğlu E, Gök AFK, Ağcaoğlu O, Yanar F, et al. (2017) Damage-control laparoscopic partial cholecystectomy with an endoscopic linear stapler. Turk J Surg 33: 37-39.
- Visser BC, Parks RW, Garden OJ (2008) Open cholecystectomy in the laparoendoscopic era. Am J Surg 195: 108-114.
- Flum DR, Dellinger EP, Cheadle A, Chan L, Koepsell T (2003) Intraoperative cholangiography and risk of common bile duct injury during cholecystectomy. JAMA 289: 1639-1644.
- Sugrue M, Sahebally SM, Ansaloni L, Zielinski MD (2015) Grading operative findings at laparoscopic cholecystectomy-a new scoring system. World J Emerg Surg 10: 14.
- Mayumi T, Okamoto K, Takada T, Strasberg SM, Solomkin JS, et al. (2018) Tokyo Guidelines 2018: Management bundles for acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 25: 96-100.
- van Dijk AH, Donkervoort SC, Lameris W, de Vries E, Eijsbouts QAJ, et al. (2017) Short and long-term outcomes after a reconstituting and fenestrating subtotal cholecystectomy. J Am Coll Surg 225: 371-379.
- Strasberg SM, Brunt LM (2010) Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg 211: 132-138.
- Hugh TB, Kelly MD, Mekisic A (1997) Rouvière's sulcus: A useful landmark in laparoscopic cholecystectomy. Br J Surg 84: 1253-1254.
- Ishizawa T, Tamura S, Masuda K, Aoki T, Hasegawa K, et al. (2009) Intraoperative fluorescent cholangiography using indocyanine green: A biliary road map for safe surgery. J Am Coll Surg 208: e1-e4.
- Lelner AI (1950) Partial cholecystectomy. Can Med Assoc J 63: 54-56.
- Bornman PC, Terblanche J (1985) Subtotal cholecystectomy: For the difficult gallbladder in portal hypertension and cholecystitis. Surgery 98: 1-6.
- Dip F, Lo Menzo E, White KP, Rosenthal RJ (2021) Does near-infrared fluorescent cholangiography with indocyanine green reduce bile duct injuries and conversions to open surgery during laparoscopic or robotic cholecystectomy? A meta-analysis. Surgery 169: 859-867.
- Henneman D, da Costa DW, Vrouenraets BC, van Wagensveld BA, Lagarde SM (2013) Laparoscopic partial cholecystectomy for the difficult gallbladder: A systematic review. Surg Endosc 27: 351-358.
- Yang J, He Z, Zhang S, Zhao X, Sun J, et al. (2020) Implementation of a simplified self-releasing biliary stent in choledocholithiasis: Experience in 150 cases. Asian J Endosc Surg 13: 195-199.
- Yachimski P, Orr JK, Gamboa A (2020) Endoscopic plastic stent therapy for bile leaks following total vs subtotal cholecystectomy. Endosc Int Open 8: E1895-E1899.
- Khadra H, Johnson H, Crowther J, McClaren P, Darden M, et al. (2019) Bile duct injury repairs: progressive outcomes in a tertiary referral center. Surgery 166: 698-702.
- Strasberg SM, Pucci MJ, Brunt LM, Deziel DJ (2016) Subtotal cholecystectomy-Fenestrating vs reconstituting subtypes and the prevention of bile duct injury: definition of the optimal procedure in difficult operative conditions. J Am Coll Surg 222: 89-96.
- Strasberg SM, Hertl M, Soper NJ (1995) An analysis of the problem of biliary injury during laparoscopic cholecystectomy J Am Coll Surg 180: 101-125.
- Fujiwara S, Kaino K, Iseya K, Koyamada N (2020) Laparoscopic subtotal cholecystectomy for difficult cases of acute cholecystitis: A simple technique using barbed sutures. Surg Case Rep 6(1): 238.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- International Journal of AIDS (ISSN: 2644-3023)
- Ophthalmology Clinics and Research (ISSN:2638-115X)